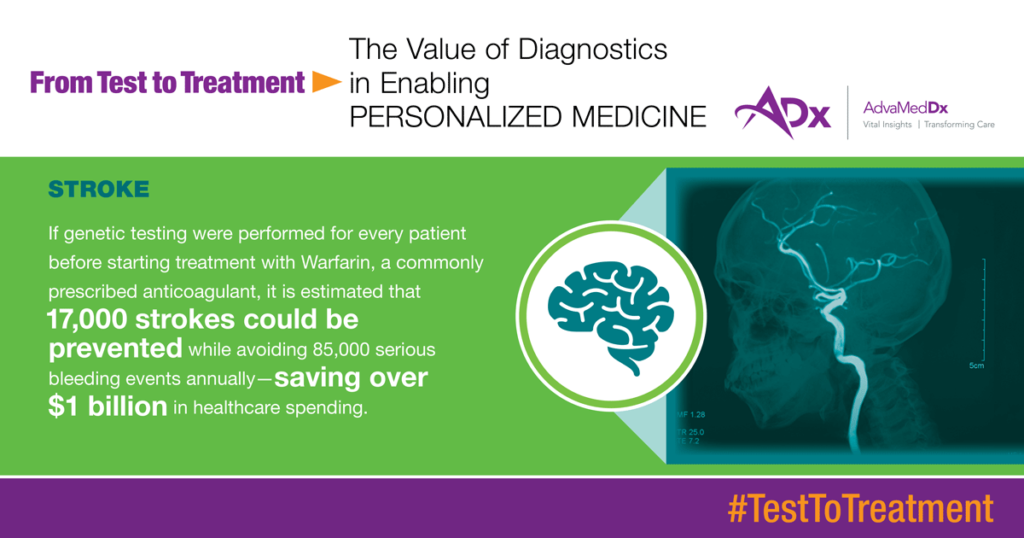
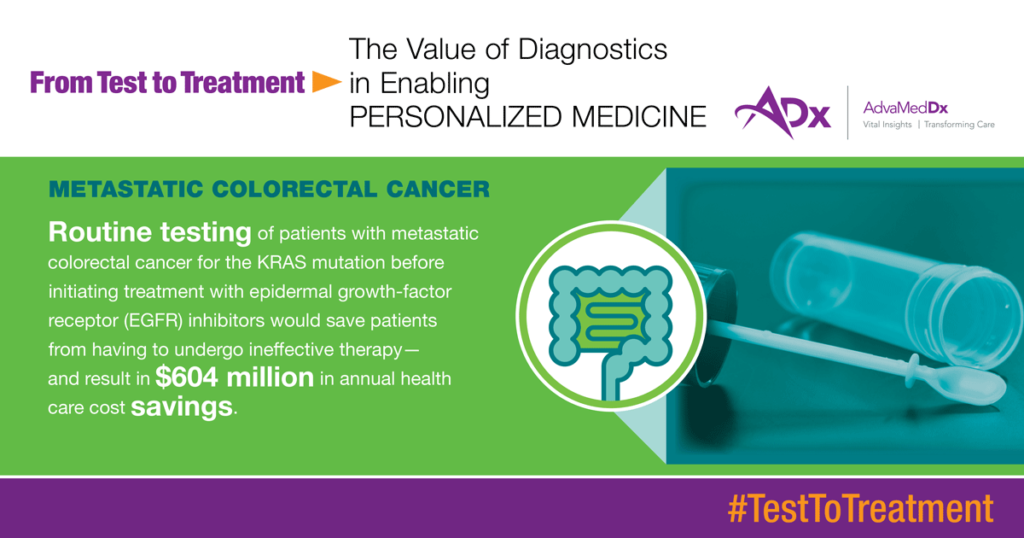
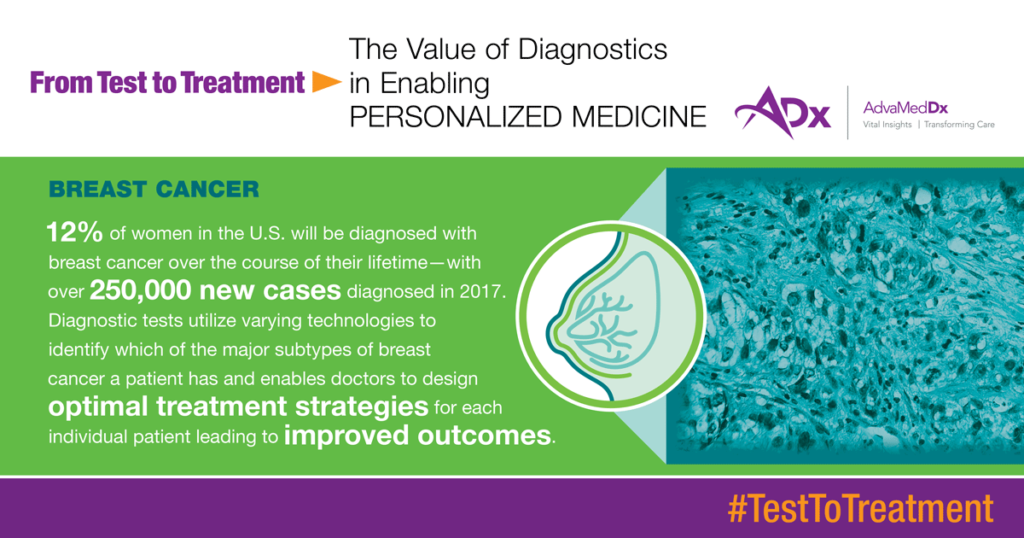
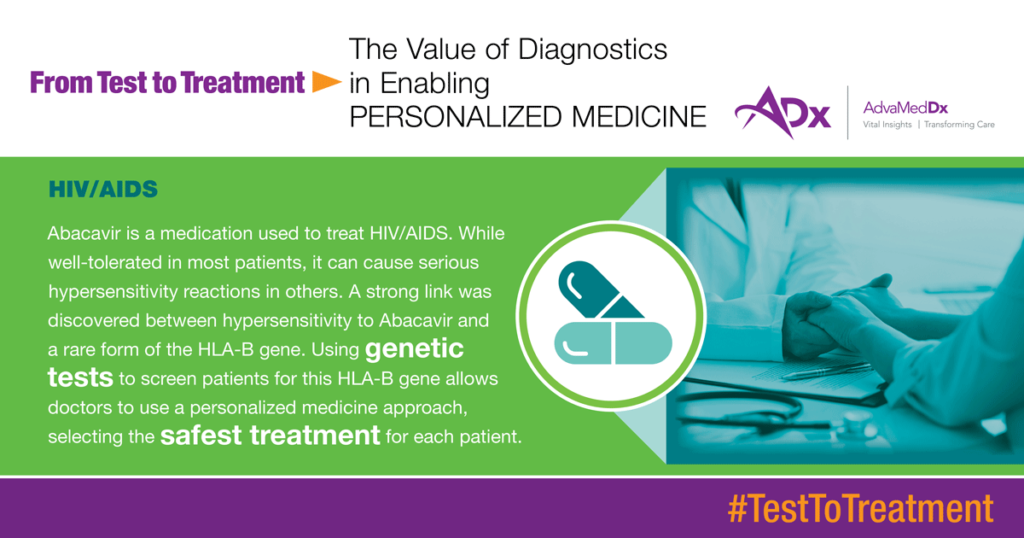
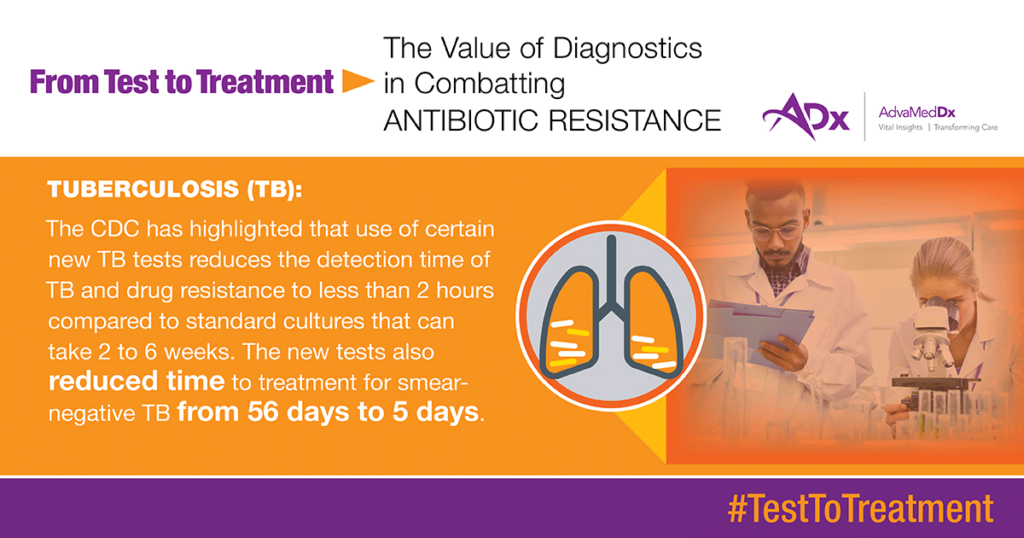
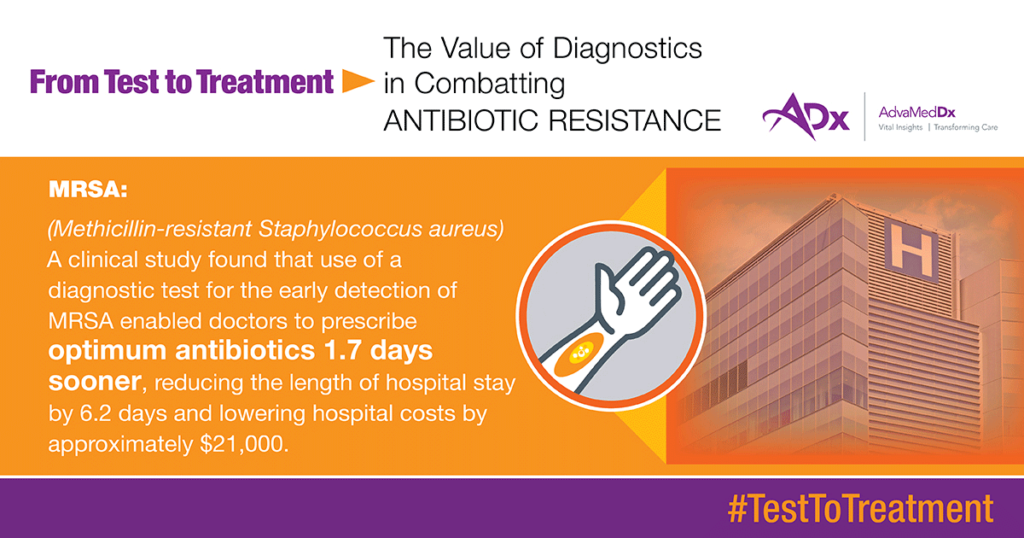
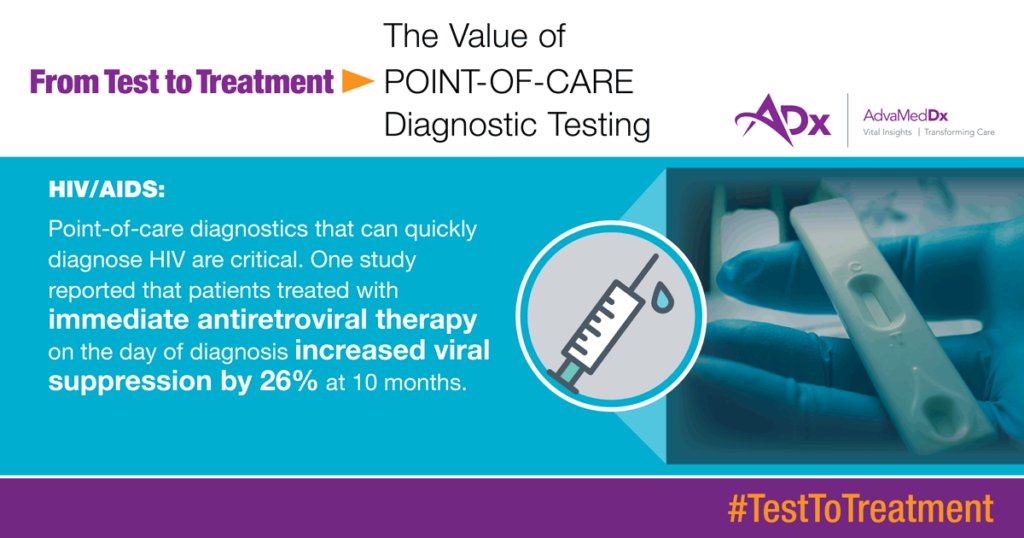
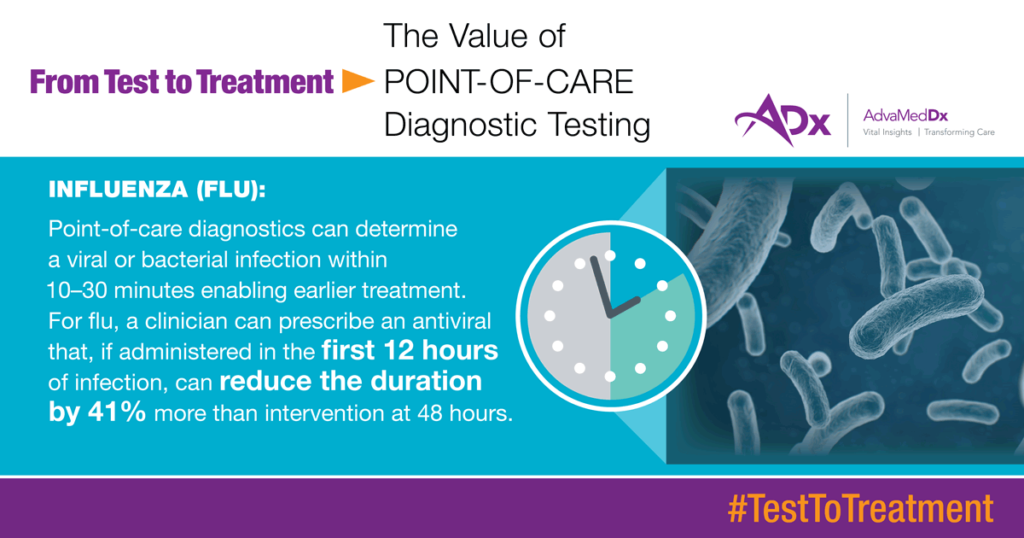
From Test To Treatment: The Value Of Diagnostics
AdvaMedDx® Test to Treatment fact sheets and social media-ready value facts communicate the value of diagnostics.
Test to Treatment fact sheets demonstrate how diagnostics are making a difference for patient and public health, including in several key disease areas. Each fact sheet includes a series of notable “value” facts, largely derived from clinical literature, which demonstrate via statistics on lives saved, cost-savings, quality of life and quality of care advances the value diagnostics bring to patient health and health care. These value facts are particularly important as healthcare stakeholders and policy makers increasingly focus on value-based arrangements, rather than fee-for-service.
Each Test to Treatment fact sheet and associated value facts are configured to be used as handouts with policy makers and stakeholders and featured on websites and leveraged via social media.